From The Wall Street Journal and The Heritage Foundation:
HEALTH INDUSTRYNOVEMBER 23, 2010.Rules Eased for Some Health Plans Text By JANET ADAMY And AVERY JOHNSON
WASHINGTON—Amid pressure from employers, the Obama administration on Monday loosened rules for bare-bones health-insurance policies. It marks one of the administration's biggest steps to peel back regulations that big business found onerous under the health- care overhaul.
McDonald's Corp. had warned regulators it might have to drop its health-insurance plans for 30,000 hourly workers unless it got an exemption for these policies, which have low premiums but also limit payments for medical costs.
Policing Insurers
Highlights of the Obama administration's new rules for insurers, based on the health law passed in March:
Beginning in 2011, insurance companies must spend at least 80% of premium dollars on medical care and quality improvement activities. This figure, known as the medicalloss ratio, is 85% for insurers in the large-group market.
Insurers that fail to meet the ratio must pay rebates to consumers by Aug. 1, 2012. The government estimates that up to nine million Americans could be eligible for rebates worth up to $1.4 billion.
"Mini-med" health plans, which have low annual coverage caps, get an exception that will make it easier for them to meet the required ratios.
Source: Department of Health and Human Services
.The administration's move underscores how businesses, after complaining loudly about the overhaul in the run-up to passage, are now winning a handful of modifications.
The change was part of sweeping new rules rolled out by the government Monday that will force insurers to spend a high portion of their premium revenue on medical care.
Consumers will reap some benefits. Insurers that don't meet the new standards will be forced to issue rebate checks, which the administration estimated could affect nearly nine million Americans, for a total payout of up to $1.4 billion.
The rules, codifying language in the health law, say insurers will be required to spend between 80% for smaller carriers and 85% for larger carriers of their revenue on medical care, a calculation known as a medical-loss ratio. That limits how much they put toward salaries, profit and other nonmedical costs.
Providers of "mini-med" policies, like McDonalds, which caps benefits at a low level, had objected that they would have trouble meeting those levels, in part because they have high administrative costs.
Experience WSJ professional Editors' Deep Dive: Agents, Employers Struggle with the MLRDOW JONES NEWS SERVICE
U.S. Issues MLR Regulations
National Underwriter Property & Casualty
Agents Anxious over MLR, 'Mini-Med' Status
National Underwriter Life & Health
Health Insurance Agents Face Bleak Future Access thousands of business sources not available on the free web. Learn More About 1.4 million Americans are covered under mini-med plans. They're typically offered by low-wage employers, who have high employee turnover and end up paying out little money in medical claims.
Under the rules disclosed Monday, mini-med policies won a reprieve for 2011 that allows them to spend half as much of their premiums on medical care as most other insurers.
Whether to give mini-med plans special treatment presented the administration with one of its thorniest choices yet since President Barack Obama signed the health-care law.
The basic McDonald's plan for newer store workers now charges a single employee $13.09 a week for a plan that tops out at $2,000 a year in benefit payments.
Democrats said eliminating plans with such limited coverage was the reason they passed the law in the first place.
But Obama administration officials said they were determined not to prompt any employers to drop their plans because of the law. "No one's going to lose their coverage," said Jay Angoff, a director at the Department of Health and Human Services.
The agency predicts that by 2014, mini-med plans will effectively disappear when the new insurance exchanges open for business, and it says the looser rules are meant as a bridge between now and then. Lower earners will qualify for new insurance tax credits.
Starting in 2014, many low wage workers will shift to getting their coverage inside new health insurance exchanges, because that's where they can tap tax credits to offset their costs. Stricter rules for the minimum benefits that employers can offer are expected to displace the plans altogether.
Neil Trautwein, a vice president at the National Retail Federation, praised the new rules and said it would help retailers and others that offer limited-benefit plans keep them in place. McDonald's said it was "pleased and encouraged" by the progress on this issue, and that it remains committed to competitive benefits and pay for those 30,000 store workers.
Mini-med plans earlier won a separate exemption that allows them to keep low limits on annual benefits. Most traditional plans are being forced to phase out such limits. More than 100 employers and other health-insurance providers received the exemption, including McDonald's, restaurant chain Ruby Tuesday and retailer Meijer.
Also, the administration this month made it easier for employers to switch carriers while retaining "grandfathered" status, which means they won't be required for the time being to follow certain new coverage mandates in the health law.
Sen. John D. Rockefeller IV (D., W. Va.) said he was "disappointed" the mini-med plans won the looser requirements, and that "their requests will be subject to close scrutiny."
The broad new rules are tough on insurers in several respects. The industry had hoped to have many expenses classified as health-care costs, which would have the effect of making it easier to hit their target. Some spending to prevent fraud or review the necessity of medical treatments will be considered administrative and can't count toward the medical costs.
"To see MLR regulations that don't acknowledge these investments in a higher-performing health system is something we remain very concerned about," said Karen Ignagni, president of America's Health Insurance Plans, the industry's trade group.
Also, some insurers hoped that they could average numbers from various states, which would mask underperforming areas. But the rule generally requires insurers to account for each state separately. One big win for insurers: The rule allows them to deduct many taxes from their total premiums before they calculate their ratios. This has the effect of boosting their numbers, and is a concession to the industry.
The pending rules have hung over the industry since March. After a booming year for profits, Wall Street expects the industry's performance to worse next year, in part because carriers that don't meet the requirements will have to issue rebates to consumers beginning in 2012.
The checks will apply largely to people who buy coverage without the help of an employer. The government said average rebates are expected to reach $164 per person.
Write to Janet Adamy at janet.adamy@wsj.com and Avery Johnson at avery.johnson@WSJ.com
A READER ON THE STATE OF THE POLITICAL DECAY AND IDEOLOGICAL GRIDLOCK BETWEEN ONE GROUP WHO SEEK TO DESTROY THE COUNTRY, AND THOSE WHO WANT TO RESTORE IT.
The Rise and Fall of Hope and Change




Alexis de Toqueville
The American Republic will endure until the day Congress discovers that it can bribe the public with the public's money.
Alexis de Tocqueville
Alexis de Tocqueville
The United States Capitol Building

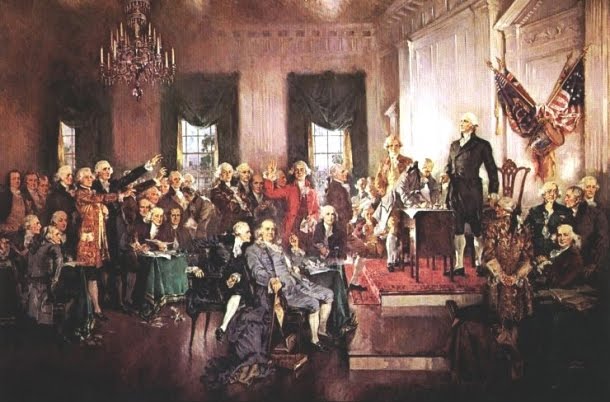
The Constitutional Convention
The Continental Congress

George Washington at Valley Forge


No comments:
Post a Comment